Approaches to Care
Including self-care, family care, community care, self-help groups
It is broadly accepted that professional health services treat only a fraction of the total burden of ill-health that may exist in a community. Last’s concept of the “clinical iceberg” (Last:1963) describes the presence of a large burden of undetected disease in the community – perhaps up to 94% of all disease. And while evidence suggests that people experience symptoms of some form or another every 3-6 days on average (Barksy and Borus, 1995), we know that people in England visit their local family practice around 8 times a year (Curry, 2015) – meaning that, for the most part, symptoms are managed informally in the community. In this section, some of the approaches to symptom management used in this context are explored.
Self-care and self-management
“Self-care” and “self-management” are broadly understood as strategies for changing the relationship between citizens and service providers into a collaborative one – with the goal of improving people’s health. The difference between self-care and self-management is often unclear. In general terms, though, self-care refers to actions by citizens who do not have a disease in order to prevent themselves from developing it; while self-management is understood as the spectrum of tools and techniques used to help people who already have a disease to manage it as effectively as possible. The range of tools used to support self-care and self-management in practice is wide, and can include the following:
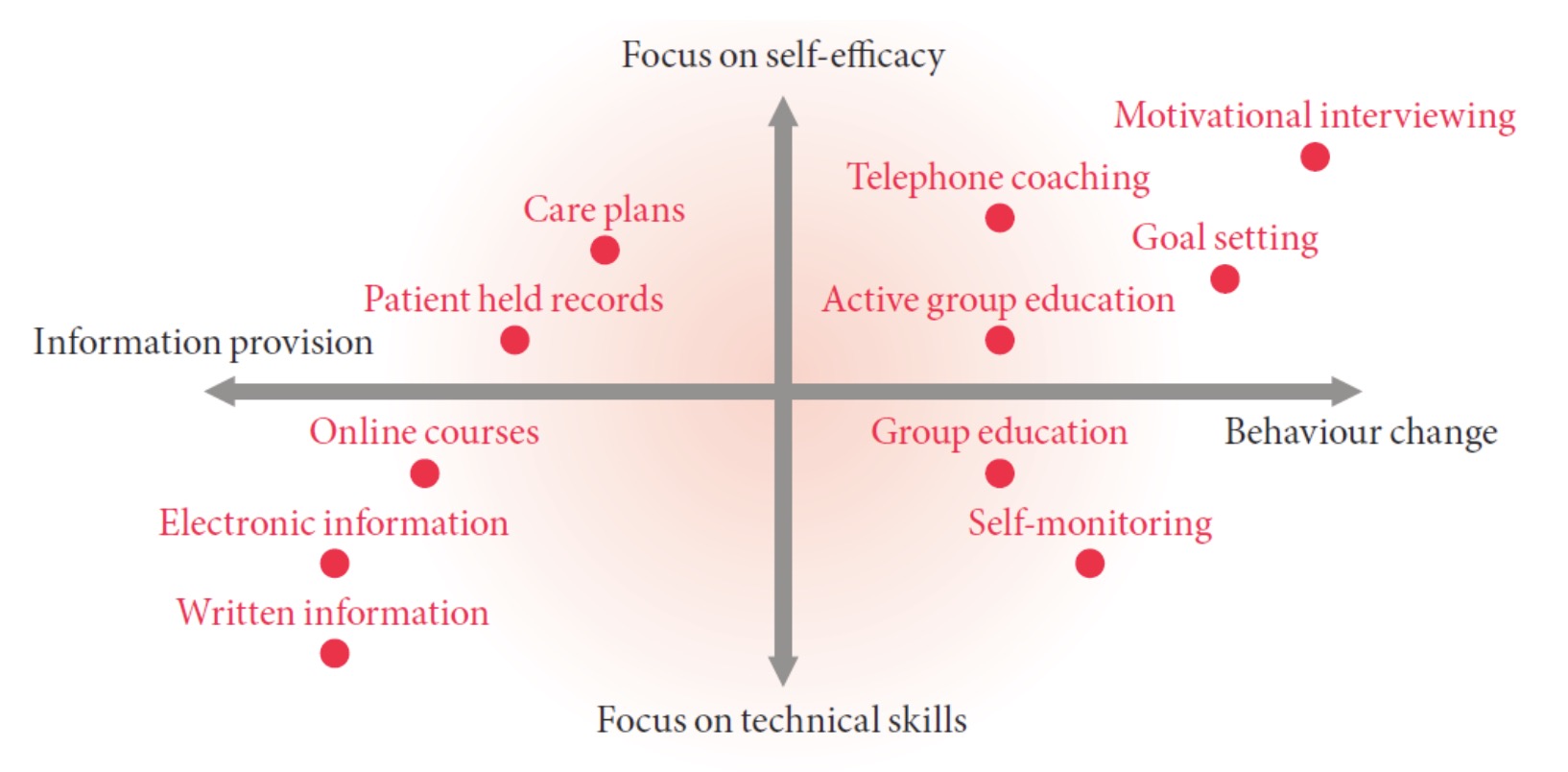
Figure 1. The spectrum of self-care and self-management approaches (source: De Silva,2011)
What sorts of care strategies are implied by these two approaches? As Figure 1 shows, strategies vary according to the degree of interaction between providers and citizens involved. At the minimalist end of this spectrum lie approaches such as information provision (e.g. in the form of leaflets) which does little to develop a citizen’s technical skills in managing their health. At the other end of this spectrum lie approaches such as motivational interviewing, an intensive form of intervention designed to improve the citizen’s ability to manage their health proactively. The means by which these interventions are delivered also varies. In recent years there has been a strong emphasis on increasing the use of technological support to self-care and self-management, including telehealth. Evidence on the clinical and cost effectiveness of these approaches is variable (Steventon et al, 2012; Totten et al, 2016).
In an increasingly straightened financial climate in many high-income countries, policymakers have shown growing interest in the potential of self-care and self-management in improving health outcomes. In England, for example, this was a central theme in the NHS’s Five Year Forward View (NHS England, 2014). Similarly, the Department for Health and Human Services in the United States identifies better self-management as one of four goals for improving the health of people with multiple chronic conditions (Grady and Gough, 2014). We encourage readers to seek out evidence on local initiatives to support self-care and self-management in their jurisdictions.
The role of informal carers and community care in the healthcare system
Large numbers of people receive social care. For instance, in England in 2015-16, just over 1.1m people out of a total population of just under 54.8m received either short or long-term support (following assessment) that was provided, purchased, or supported by CSSRs (Councils with Social Services Responsibilities) (NHS Digital, 2016). Reductions in the scale and scope of care services offered to citizens in the community have been a major feature in the UK since 2010 (Ismail et al, 2014).
However, this focus on community care services provided by local authorities does not give the whole picture of care provided for people with chronic illness, and other disabilities outside the hospital. An important distinction needs to be between care that is provided in the community (carried-out by the Health and Social Services), and care by the community or informal care. The latter is care provided primarily on the basis of kinship obligations between members of the immediate family.
The realities of community care policy have meant that informal care provision remains predominant. In England the average number of contact hours with clients receiving home care provided by health and social care professionals rose steadily from 6.6 hours per week in 2008-9 to 7.6 in 2013-14 (although it should be noted that overall, the number of people in receipt of home care has declined, so greater care provision probably reflects higher intensity need for support in the home care group over time) (Health and Social Care Information Centre, 2014). This clearly means that informal carers continue to provide the bulk of the support required by clients. In 2015-16, some 387,000 carers were in contact with their local authority, just over 80% of whom received direct support from that body to deliver care to relatives – but this likely underestimates the total number of people providing informal care. (NB 'Home Care' is defined as those services which assist the client to function as independently as possible and/or continue to live in their own home. Services may involve routine household tasks within or outside the home, personal care of the client or respite care in support of the client's regular carers. It excludes services other community-based services such as day care, meals, transport and equipment (NHS, 2005)).
The needs of informal carers have historically received scant attention from both researchers and policymakers. It was not until 1985 that the first large-scale survey of informal carers was carried out by the government (OPCS, 1988). Up until that time, most research had focused on the needs of those requiring some form of physical or social care, whilst the role of their carers had received relatively little treatment. This survey revealed that 14% of the population over 16 were ' looking after, or providing some regular service for someone who was sick, elderly or handicapped.'. Subsequently in 1997, the ONS carried out a much larger survey of informal carers which was published within the General Household Survey (ONS, 1998). The findings broadly replicated the previous studies, in that one adult in eight was found to be providing informal care, and that one in six households contained a carer (estimated 5.7 million carers overall in the U.K).
However, it is was recognised that much more reliable information was required regarding the numbers of specific caring activities, and so a question was included in the 2001 census to address this continuing shortfall in knowledge. The most recent census for England and Wales in 2011 found that there were 5.8 million unpaid carers of which,
- 64 % (3.7 million) provide care for up to 19 hours per week
- 13% (0.78 million) provide care for 20 to 49 hours per week
- 24% (1.4 million) provide care for 50 or more hours per week
These figures reflect a steady increase in the highest intensity of support by informal carers (i.e. 50 or more hours per week) from the 2001 census (White, 2013).
Policy Assumptions regarding the role of Informal Carers
The policy of community care makes a number of explicit normative assumptions about where the responsibilities for care lie. Some of these assumptions are discussed below:
- The relationship between the responsibilities of the State and the Family:
'Community care' for the vast majority of those who require care in their own homes, has always meant the ‘informal care’ given to them by their family members – a fact often overlooked at policy level. In England, the introduction of the Community Care Act did address for the first time the issue of who actually performed these caring tasks. There is now an acknowledgement by UK governments of their responsibility to provide, through local authorities, domiciliary services, respite care and day care as supplements to family care.
- A changing role for the family? There is a commonly expressed and essentially moralistic view that the problem of meeting the needs of dependent groups in the community arises because we no longer care for our family members in the way that occurred automatically in the past. This view is predicated on an assumption that the role and function of the family has dramatically changed over the last hundred years. The main change being a shift from the ‘extended family’ taking responsibility for the care of its sick and elderly members, to the ‘nuclear family’ of the mid-twentieth century, which had many of these caring functions taken-over by systems of state welfare. This however is a simplistic reading of the history of the family. It ignores the fact that the major change in the twentieth century was not a shift towards the nuclear family household group, but an absolute decline in the size of families, and a greater geographical dispersion of households containing related people. Crucially, the demographic shift towards people living longer has resulted in an increase in the number of dependent elderly people. Interestingly, as long ago as 1911, 5% of the elderly population were in some type of institutional care, today that proportion is virtually identical (although absolute numbers are very much higher).
- Caring as 'Women’s Work' Tied in with the expectation that families would take responsibility for providing care is a general assumption about the role and responsibilities of women in society. The assumption that women are expected to undertake the major role in caring for dependents (including pre-school children, children with disabilities, parents and husbands with disabling illnesses, etc), in many ways remains in many areas of government health and social policy-making. However, as Marian Barnes (1998) points out, demographic changes, shifts in employment patterns, as well as changes in what are perceived to be acceptable divisions of labour between men and women, have meant that the availability of female family members continuing to take on this role in the future cannot be confidently assumed.
- Culture and Caring: There has been a tendency by policy makers to assume that caring for dependent relatives is not a ‘problem’ within ethnic minority communities. This reflects a stereotypical assumption regarding the existence of the extended family (particularly as regards Asians), which does not reflect the reality of the situation, and can manifest itself in inequity in formal care service provision.
The role of self-help groups
The rise of self-organising groups of people in civil society offering mutual support to one another is a central feature of the health landscape in many countries today. Self-help groups (SHGs) address a vast range of perceived needs, and have a particular track record in the areas of mental health and substance misuse. Their functions can include provision of information and facilitating contact between individuals with the same health condition for purposes of support. But they have been seen by some as part of a broader trend towards consumerism in the health sector (Borkman, Munn-Giddings, 2008). Commonly given examples of SHGs could include groups such as Alcoholics Anonymous (where participants often meet in person) or Mumsnet (where mutual support is provided predominantly online) – but many large third sector organisations now have member networks providing varying degrees of mutual support.
SHGs have also, however, come to assume an increasingly important political role over the past 30 to 40 years, in both lobbying for political and sometimes legislative recognition of their particular interest or patient group’s needs, and raising funds for their activities and sometimes for health research. This change brings with it important challenges, particularly in regard to independence. One large study of patient groups from the UK found some evidence that they could influence or reform public policy, but that this was heavily dependent on resources, leadership and the ability to form meaningful alliances with other groups. There may also be adverse consequences to this engagement – including the potential for manipulation by government, health professionals or corporate interests in the health sector (Baggott and Jones, 2014)
@ I Crinson2007, S Ismail 2017
