PLEASE NOTE:
We are currently in the process of updating this chapter and we appreciate your patience whilst this is being completed.
Concepts of health, wellbeing and illness, and the aetiology of illness: Section 10: The role of social, cultural, psychological and family relationship factors in the aetiology of disease and illness
This section covers:
1. Social factors in physical and mental health
2. Psychological factors: Stress and health behaviours
3. Cultural factors and lay health beliefs
4. Family relationships and social support
The aetiology of illness and disease is influenced by a variety of social, cultural, psychological and interpersonal factors. These factors interact to contribute to the causes and consequences of ill-health, and how these are experienced and interpreted by individuals.
1. Social factors in physical and mental health
Social influences on health are discussed in Section 9. Early life experiences are known to be key determinants of mental and physical health. The Adverse Childhood Events scale identifies experiences in childhood associated with increased risk of poor health in adult life, including domestic violence, abuse, deprivation and parental divorce.[1] However, it is also recognised that not all people who experience adverse events in their early childhood will go on to have health problems. Factors associated with resilience during the formative years, such as feeling loved or having an adult in the household who cares about the child’s education, can mitigate the effects of adverse experiences. Throughout the life course, social support at a number of levels is crucial to enabling individuals to manage difficult or stressful circumstances (see Family relationships, social support and social integration below).
Among working age adults, employment is one of the most strongly evidenced determinants of health – not just in terms of the social and health consequences of employment or unemployment, but the impact of the work itself. The Whitehall studies, which began in 1967, have long established a social gradient in work and health, with lower employment status associated with increased morbidity and mortality (see Marmot, 2010). Lower paid, lower skilled workers are more likely to take absences and to fall out of work altogether due to ill-health (Black & Frost, 2011); insecure, low-quality and low-status work reduces the amount of control and support people have at work, which in turn has detrimental effects on physical and mental health (Marmot, 2010).
2. Psychological factors: Stress and health behaviours
Stress is the most widely discussed psychological factor in health, particularly in relation to work. It is estimated that one in six workers per year in England and Wales is affected by anxiety, depression and unmanageable stress. In 2011/12 workers in Great Britain lost 10.4 million working days to stress, with an average of 24 days per worker (HSE, 2012). However, stress is a complex and multi-faceted issue. Though its implications for mental health are well-known, stress can also exert physical effects (see The relationship between mental and physical health, Section 3).
What constitutes ‘stress’ (and subsequently ‘stressors’) is in itself complicated due to the strong subjective element, but a broad definition of stress is that it results from a lack of ‘fit’ between a person and their world, leading to physical or mental illness (Cassidy, 2001). Within the context of the working environment, this fits the Health and Safety Executive’s (HSE’s) definition of work-related stress as developing because a person is ‘unable to cope with the demands placed on them’.[2] It is also consistent with the key aspects of work-related stress identified by the Whitehall II study, which found that imbalances in effort/reward and demand/control had the greatest impact on stress. The usefulness of stress terminology has nevertheless been questioned; it has been asserted that it is now so widespread that it can be used to ‘explain everything and as a result explain nothing’ (Cassidy, 2001). It is important to bear in mind that being affected by stress does not necessarily result in absenteeism, which has traditionally been used as an indicator of poor health among workers (Johns, 2010; Sanderson & Cocker, 2013), but instead may be masked by presenteeism, i.e. being at work whilst one is ill. A Swedish workforce Study (Aronsson et al, 2000) found that levels of presenteeism were highest among people working in care, welfare or educational capacities, suggested that a sense of social responsibility plays a part in reluctance to take time off sick. More recently in the UK, there has been increasing concern around the rise in ‘zero hours’ contracts and their impact on presenteeism.
Psychological factors influence not just the experience of health and illness, but also health behaviours. This influence can be reactive, e.g. drinking more due to stress, or proactive, e.g. making decisions about smoking cessation based on beliefs about health and belief in one’s own ability to make changes. Perceptions of factors such as risk, susceptibility, costs, consequences, control and confidence in ability to make changes all predict behaviours relating to health, and can help to understand lay concepts of health (see Cultural factors and lay health beliefs below).
3. Cultural factors and lay health beliefs
The findings of sociological research into lay health beliefs which focus on discovering the rules and meanings that different social groups use to order their lives and make sense of their experience of health and illness have been of great value to clinicians. Such findings demonstrate the sophistication and complexity of lay beliefs about health, and point to the need for health professionals not to treat patient views as merely 'incorrect knowledge' and so improve the patient-professional relationship.
"Ordinary people develop explanatory theories to account for their material, social and bodily circumstances. These they apply to themselves as individuals, but in developing them they draw on all sorts of knowledge and wisdom, some of it derived from their own experience, some of it handed on by word of mouth, other parts of it derived from highly trained practitioners. Thus lay explanations go beyond common sense, in that explanations beyond the immediately obvious are included” (Stacey:1988:142)
Most sociological studies of lay health beliefs agree that public conceptions of health and illness vary according to the immediate material and social circumstances in which people find themselves. These circumstances can act to constrain the possibilities for action to change an 'unhealthy lifestyle'. Nevertheless, health promotion strategies have in the past assumed that persuading people to adopt healthy 'lifestyles' was largely about changing individual attitudes. However, as the work of Davison et al (1991) has shown, to oppose so-called 'lifestylism' (the awareness of the causes and possible ways to avoid illness through behaviour change) with 'fatalism' (life is full of random chance events outside of my control), is to misunderstand the real situation for most people. In their fieldwork in South Wales, the researchers found that:
'only very few informants whose belief in randomness led them to deny or ignore the possible benefits of lifestyle change. Rather, the recognition of a pervasive uncertainty in the field of illness and death existed side by side with a common-sense approach to taking appropriate care' (Davison et al:1991:106)
At least in part, one consequence of such lay beliefs research was to bring about some shift of focus in the health prevention strategy of the government. The New Labour government Public Health White Paper, Saving Lives: Our Healthier Nation (1999), for example explicitly recognised that:
'Past health strategies have tended to focus excessively on lifestyle issues. People were treated as passive recipients of information and services, rather than active partners. This contributed to a widening of the health gap: we now know that the better off are more likely to act on health information to change behavior. Although people may know what affects their health, they can find it difficult to act on what they know, setting up a downward spiral of deprivation and poor health' DoH: 1999:3.2 / 4.10).
In 2001, in recognition of the cumulative sociological evidence of the potential for dissatisfaction and misunderstanding resulting from the different perspectives of treatment and care existing between doctors and patients, the Department of Health set out guidelines for a new approach to doctor-patient relations that it termed 'The Expert Patients Initiative' (DoH:2001). This shift in clinical focus is all about formally recognising the intimate (and rational) knowledge and experience that patients have of their illness, and encouraging patients to take an 'active role in their own care'.
Sociological research into these lay health beliefs spans a thirty-year period, Table 2 below is an attempt to summarise the main findings and give examples of how such beliefs play out in the real world ('indicators').
Table 2: Summary of Sociological Studies of Lay Health Beliefs (Crinson:2007)
|
CONSTRUCTS |
INDICATORS |
|
Health as functional capacity (Blaxter:1982) This broad notion would also include the notions of ‘health as the absence of disease' (as not ill) as well as ‘health despite disease' (Blaxter:1990). Largely a working-class conception, but also held by the elderly, particularly those in poor health, who were less likely to define health in terms of illness. |
|
|
Health as emotional wellbeing (MacInnes & Milburn:1994) Closely linked to health as energy / vitality (Blaxter:1990). d'Houtaud & Field (1986) saw this as essentially a middle-class concept. |
|
|
Health as reflecting lifestyle, including a moral dimension (MacInnes & Milburn:1994) Closely linked to health as ‘healthy' behaviour, the `healthy life' (Blaxter:1990). |
|
|
The notion of `candidacy' Utilised in lay explanations of relative risk of disease and efficacy of preventive health behaviours. Constructed from appearance or circumstances surrounding an event, i.e. the onset of illness. Can support or challenge biomedical aetiology (Davison, Davey Smith & Frankel:1991) |
|
|
Conceptual duality of health Endogenous health / exogenous illness (Herzlich:1973) |
|
|
Theorising the body as physical capital or the ‘commodification of the body' (Bourdieu :1977). Working class having an instrumental relation to body; Middle class seeing the body as a ‘personal project'. |
|
Nevertheless, while it is recognised that individuals have a key role in managing their own health and should be respected as active partners in their care, it is equally important to act upon the structural socioeconomic factors underlying health beliefs and behaviours. Despite increasing acknowledgement of the key role of the wider determinants of health, there remains a tendency for health promotion policy initiatives that start off with an upstream or social determinants approach to drift downstream to largely individual, lifestyle factors, with investment at the individual rather than population level (Carey et al., 2016; Popay et al., 2010). This phenomenon has been termed ‘lifestyle drift’, and is evident in both Saving Lives: Our Healthier Nation and the Choosing Health: Making Healthy Choices Easier white paper that followed.
Models of 'help-seeking' or illness behaviour
The sociological approach of Zola (1973) found that people`s responses to symptoms were contingent upon their cultural values / beliefs concerning health. That is, their perception of what is 'normal'. Accordingly, the decision to seek professional medical help was either promoted or delayed by social factors. Zola`s (1973) model (set out in Figure 5 below) identified five different types of incident which ‘triggered' the decision to seek medical care, incidents which threaten people`s notions of normality.
However, the interesting feature of the model is that the decision to seek help does not necessarily lead directly on a path to the medical professional. People draw upon what is termed a 'lay referral' system which includes family, friends and the local community - so for example a young mother faced with a baby that is continually crying may choose not to go directly to the GP because they may be afraid that they will be categorised as an 'anxious mother' and so instead approach their own mother or other mothers with older children for advice. People increasingly are engaging in 'self-medication' as generic drug treatments become more widely available over the counter. They may also be one of the hundreds of thousands of people each year who opt for what is loosely termed 'alternative' medical care; now a multi-billion pound industry in Britain.
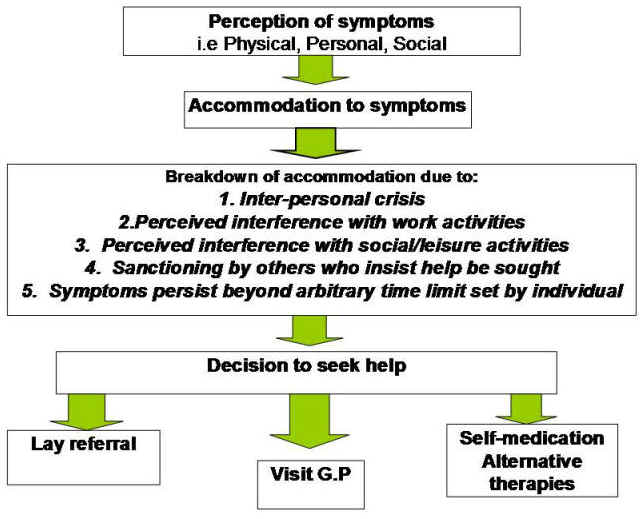
Figure 5 : Zola's Help-Seeking Model
Despite the influence of such help-seeking models, health policy over the past two decades has generally been less concerned with illness behaviour than with developing strategies to promote health maintenance (health behaviour). Here both social psychological models and sociological approaches to understanding lay health beliefs have been applied in attempting to bring about health and lifestyle change.
4. Family relationships and social support
Social science research has suggested that the relative quality of individual and group social relationships serve to act as psycho-social mediators in health outcomes. The quality of these relationships is seen to reflect the degree to which individuals possess or have access to a wide set of social networks and a shared set of social norms (see Section 11). Sociologists recognise these factors as being key characteristics of a cohesive society.
The findings from a wide range of epidemiological studies have concluded that social and psychological stress is one of the major factors impacting upon an individual's ability to maintain their health (Wilkinson 1996; Marmot and Wilkinson:1999; Marmot and Wilkinson:2001). Sociological and social psychological research has concluded that whilst we all experience such stresses or 'life events', their effects are magnified for those individuals and social groups that have limited social support, a limited ability to control one's social situation / environment, poor social networks, and low levels of social integration.
Social Support
This construct focuses attention upon the importance of inter-personal relations. It encapsulates notions of emotional support, instrumental aid, information giving and personal appraisal. However, as a construct it can lack a certain amount of clarity.
Social psychologists see sources of social support as deriving from social networks. The importance of these networks lies in their function as a 'buffer' against the negative impact of stressful life events - helping people to adapt. The main source of social support in chronic illness, for example, comes from the family. Brown and Harris's (1978) classic research into clinical depression amongst working class women recognised that differential availability of social support was a critical factor in a person's relative 'vulnerability' to stressful life events. They saw social support acting through what they termed intimacy, serving as a powerful mediator between the stressor (provoking agent) and the onset of illness (depression).
The importance of social support for health is highlighted in the Marmot Review (2010), with loneliness and social isolation linked to premature mortality and increased risk of depression. Strong social networks are associated with increased happiness and health, and better recovery from illness; in addition, social participation may act as a protective factor against dementia and cognitive decline. People living in more deprived areas are more likely to severely lack social support compared to those in more affluent areas (pp. 136-137), which relates to social cohesion and capital (see section 11).
The lack of social support as negatively related to health and health inequalities is recognised as a public health issue by the Department of Health. In 2013/14 the Adult Social Care Outcomes Framework was updated to include a measure of social isolation, in order to identify where older adults are more likely suffer from loneliness and target care appropriately. No Health Without Mental Health also emphasises the importance of social inclusion and support to improve mental health in citizens and communities. Figure 6 illustrates the relationship between lack of social support and mental health problems, demonstrating how stresses associated with poverty such as social isolation and material deprivation may push already vulnerable individuals into addictive behaviours and psychosis. Figure 7 shows the results of a meta-analysis by Holt-Lunstad et al. (2010), whose review of 148 studies found that with the exception of smoking, social support was more strongly associated with mortality risk than any lifestyle factor.
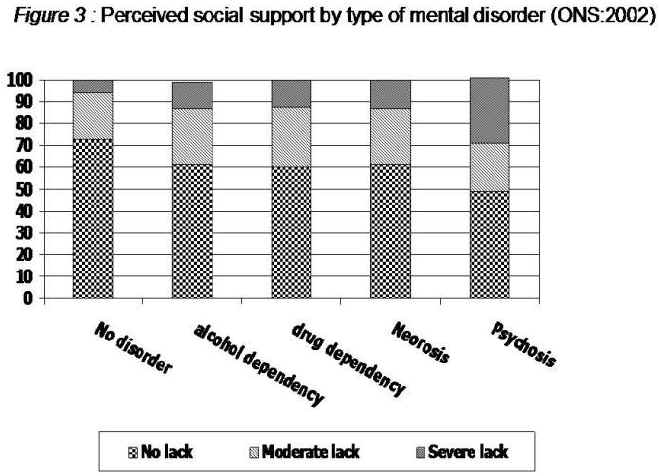
Figure 6: Perceived social support by type of mental disorder (ONS, 2002)

Figure 7: Comparison of odds (lnOR) of decreased mortality across several conditions associated with mortality (Holt-Lunstad et al., 2010)
© I Crinson 2007, Lina Martino 2017
[2] HSE. Work related stress. http://www.hse.gov.uk/stress/furtheradvice/wrs.htm
