PLEASE NOTE:
We are currently in the process of updating this chapter and we appreciate your patience whilst this is being completed.
Concepts of health, wellbeing and illness, and the aetiology of illness: Section 9: Explanations for various social patterns and experiences of illness including: differences of gender, ethnicity, employment status, age and social stratification
This section covers:
1. The social model of health
2. The Epidemiological transition and the rise in life expectancy in developed societies
3. Social determinants of health in contemporary society
4. The persistence of social inequalities in health
1. The social model of health
Dahlgren and Whitehead’s (1991) framework illustrating the wider determinants of health is the most effective representation of how individual, social, economic and cultural factors impact on inequalities and inequities in health and illness (see Figure 2). At the centre, susceptibility to mental illness may be determined by individual risk factors such as age, sex or genetics. These are influenced by lifestyle factors, which in turn are determined by social and community networks and relationships. These are impacted on by living and working conditions, which are determined by the broader socioeconomic, cultural and environmental context. Health beliefs (e.g. health locus of control and self-efficacy; see section 10) are not an explicit component of this model, but health psychology theory and research suggest that they are crucial in how we process and act upon health information, which has implications for how resilience, susceptibility and response to mental ill-health are developed.

Figure 2: Social model of health (Dahlgren & Whitehead, 1991).
Significant differences in mortality and morbidity rates continue to exist between income groups and social classes in most developed countries. This salient fact serves to remind us of the continuing importance of social and economic determinants of health. Certainly, there is little doubt that the low standard of living and persistence of absolute poverty in the developing world are the key determinants of health in these countries; as they were in the early stages of development of modern industrialised societies. In developed countries, relative rather than absolute poverty is the main driver of inequality; this is discussed in more detail in Section 9. The Black Report suggested four theories (artefact, selection, behavioural/cultural and structural) as to the root causes of health inequalities, concluding that structural theory provided the best explanation.
The knowledge that our life processes are socially and economically structured as least as much as they may be genetically determined, turns the exploration of the determinants of population health into a social science:
'Medical science can address the biological pathways involved in disease, the pathology and the opportunities for treatment, but in so far as health is a social product and some forms of social organisation are healthier than others, advances in our understanding of health will depend on social research ' (Wilkinson:1996:13).
‘Inequalities in health arise because of inequalities in society – in theconditions in which people are born, grow, live, work and age.’ (Marmot, 2010)
It is important to make the distinction between inequalities in health, which are unavoidable differences that exist due to factors that cannot be changed, and inequities in health, which are avoidable and a matter of fairness and social justice. There can be some confusion between what is avoidable and/or fair, and what is not (see subsection 3 below).
2. The Epidemiological transition and the rise in life expectancy in developed societies
In the 20th century, life expectancy in developed societies increased at the rate of two to three years added to life with each decade that passed. These increases in population life expectancy have primarily come not as a result of people living longer (although there have been significant increases), but from the reduction in infant mortality followed by reductions in childhood mortality. As a result, a much higher proportion of the population now lives to old age.
The notion of the ‘epidemiological transition' is used to denote the historical change in developed countries from predominantly infectious diseases as the primary cause of death to degenerative diseases. This change is reflected in the levelling-out in the curve of life expectancy compared to increases in per capita income in developed countries in the mid to late twentieth century. When levels of economic growth in a society are such that a general rising in the standard of living and income occurs, in tandem with a process of qualitative technical change and development, then we find that general levels of health and life expectancy begin to rise. This transition is also marked by a change in the social pattern/distribution of diseases. What were seen as ‘diseases of affluence' in the early twentieth century, such as coronary heart disease, stomach ulceration, stroke and obesity, became more common among the poorer sections of these affluent societies reversing their previous social distribution (Wilkinson:1996;43-47).
3. Social determinants of health in contemporary society
Examining health from a societal perspective rather than that of the individual produces a very different view of the determinants of health. This is not necessarily because the individual determinants of health identified in clinical studies do not add up to become the societal determinants; rather:
'What really moves the health of whole societies, adding to or subtracting from the sum of total health, may be factors which account for only a very small part of the individual variation in health and so escape detection ' (Wilkinson:1996,16.)
Social explanations for this variation include biological (e.g. age), behavioural (e.g. smoking) and social factors (e.g. unemployment). These factors do not operate in isolation, but interact with the wider context to influence health. Another explanation is artefact, which is when observed differences are due to biases in data collection or categorisation; for example, a reduction in child poverty may be an artefact of changes in how child poverty is defined.
Gender
Gender accounts for a number of inequalities and inequities in health status, and is the characteristic where the two concepts are most often confused. The fact that life expectantly is generally and consistently lower for men than women is widely accepted as an unavoidable inequality in health due to fixed differences between genders, but when many of these differences are unpicked it is clear that social factors play an important role. Inequalities relate to diseases that affect men and women differently due to physiological differences, e.g. only men can get prostate cancer, and women are more likely to get breast cancer. Inequities arise from differences in psychological, behavioural and social characteristics that cause men and women to behave and be treated differently.
A number of mental disorders are more common in women: for example, unipolar depression, which is one of the leading causes of disability globally, is twice as common in women.[1] Explanations throughout history tended to focus on hormones as the cause, portraying women as victims of ‘raging hormones’ (see Walker, 1997). More recently, however, biopsychosocial explanations have considered hormonal factors within their social and cultural contexts. The role of women in Western society has undergone major transformations throughout the last century, yet the advantages of increased gender equality appear to have come at a price. Female roles have been added to rather than altered, resulting in ‘role conflict’ among many women (Unger & Crawford, 1996). Whilst a woman in paid employment will be expected to display full commitment and competence in her position, showing equality in terms of the traditional male model, she will also be expected to follow the traditional female model by giving highest priority to family, which may subsequently have deleterious effects on physical and psychological wellbeing. Studies have revealed that decreasing role strain within marriage reduces the incidence of women’s mental and physical disorders (e.g. Helson & Picano, 1990). Lesbian relationships, which are characterised by less stereotyped roles and more equal distribution of power and workload, have been linked to higher levels of relationship satisfaction (Greene & Herek, 1994).
Social constructs of gender roles can also have detrimental effects on the health of men. Farrell (1993) argues that the notion of male power is a myth within modern Western societies, as constructs of masculinity that position men as breadwinners, protectors and defenders lead to a different, but equally damaging, set of health and social problems. For example, lung cancer has a higher incidence in men than in women,[2] which can largely be attributed to differences in smoking and occupational risks (e.g. exposure to asbestos). Men are also more likely to die from violence or suicide, particularly those who are younger and live in more deprived areas.[3] Differences in health-seeking behaviour can help to account for these inequities, and also for apparent discrepancies in disability and death: while life expectancy is lower for men, rates of illness tend to be higher among women. This is believed to be partly an artefact of increased reporting among women, who are more likely to seek help for health concerns (see Bogle, 2013).
Ethnicity
As with gender, it can be difficult to separate inequalities from inequities, and biological factors from social and cultural. Certain conditions are more prevalent among certain ethnic groups due to genetic factors. For example, the risk of skin cancer is highest among people with fair skin that burns easily, and lowest among people with naturally dark brown or black skin.[4] Other conditions show more complex relationship with ethnicity, and artefact is common in the reporting of ethnic differences in health status. In England, for example, black and minority ethnic (BME) groups are more likely to live in deprived areas compared with the white British majority, with some regions showing greater discrepancies than others; ethnic disparity is greatest in the Midlands, and smallest in the South (Jivraj & Khan, 2013). As a result, the social factors that affect BME populations as they would any other (i.e. imbalances in socioeconomic status, wealth and poverty) are misleadingly attributed to racial or ethnic differences.
This tendency may further perpetuate ethnic inequities by stigmatising certain groups and resulting in discrimination, whether direct or indirect (see section 5). Racism impacts directly on health through causing stress and social isolation, but there may also be indirect effects of health services being less accessible to people from some minority groups. For example, new migrants to the UK or first-generation immigrants may experience barriers to attendance relating to language.
The relationship between ethnicity and health is nonetheless complex, with some social factors linked with cultural practices within different ethnic groups. The increased prevalence of Type 2 diabetes and cardiovascular disease among people of South Asian origin has been attributed partly to biological factors, with abdominal fat and higher BMI presenting a greater risk at lower thresholds than for other ethnic groups (Gujral et al., 2013). However, these differences can be partly explained by social and cultural factors such as diet and lifestyle. The traditional South Asian diet is high in carbohydrates, trans fats and saturated fats, and recent decades have seen an increase in the consumption of animal products, sugars and fats (see The Epidemiological transition above). Among South Asians who migrate to Western countries, the risk may be exacerbated by increased consumption of non-traditional foods, such as margarine, juice, chips, soft drinks, alcohol and fast food (see Gujral et al., 2013). First-generation immigrants are more likely than second- or later-generation immigrants to benefit from ‘cultural buffering’ against unhealthier lifestyles, as they are more likely to retain aspects of the cultural context they grew up in. This contributes to a phenomenon termed the ‘healthy migrant effect’ (see Domnich et al., 2012). Migration may also result in a loss of social capital due to isolation from family and social networks (see Section 11), which may be exacerbated by the experience of discrimination.
Age
Age influences health across the life course, not just in terms of differences in mortality and morbidity, but also in the social experiences and determinants of health. Among older people, who account for the majority of people with long-term limiting illness or disability, poverty is the greatest predictor of poor health; this reflects the carrying of social disadvantage throughout the life course and into old age (Draper & Fenton, 2014; Grundy & Holt, 2001;). While ageing may increase the risk of many diseases (e.g. types of cancer), it is assumed that poor general health is an inevitable consequence of ageing, and experiences of chronic illness or disability are often dismissed as being due to ‘old age’. However, social factors such as differences in access to treatment may also contribute to worse health outcomes in older people; for example, poorer survival from cancer among older people may be due at least in part to under-treatment compared with younger patients (Macmillan, 2012). It has been argued that the use of quality-adjusted life years (QALYs) to assess the potential costs and benefits of treatment are ‘inherently ageist’, because they may disadvantage older people when comparisons are made with younger groups with more QALYs to gain from treatment (Harris, 2005). Stereotypes about the health needs of older people may also reduce availability of services, e.g. a tendency to focus on dementia means that other long-standing mental health issues can be neglected in older groups. Negative expectations of health in older age may also influence health behaviours (e.g. Goodwin et al., 1999).
While it is older age that tends to be the focus of age differences in health status, a number of conditions are more common in younger people, including STIs. The epidemiology of STIs suggests that young people, and especially young women, may be more vulnerable to having unsafe sex. This may be due in part to females being more likely to have had their first sexual intercourse by age 16 (Hawes et al., 2010) and to have older male partners (e.g. Mercer et al., 2006). It has also been suggested that young people often lack the ‘skills and confidence to negotiate safer sex’ (NICE, 2010). Gender inequalities in STI risk have been linked to power relations between men and women: for example, intentions to use condoms are more strongly correlated with actual behaviour in men than in women (Abraham et al., 1996), suggesting that young women may face more barriers to negotiating condom use.
Employment status
Waddell & Burton’s independent review (2006) concluded that being in work is generally beneficial to physical and mental health and wellbeing. For common health problems, such as mental illness, cardio-respiratory conditions and musculoskeletal conditions, encouraging and supporting people to remain in/return to work can improve quality of life and wellbeing on a number of levels: therapeutically, by promoting recovery and rehabilitation; materially, by reducing poverty; and socially, by enabling independence and promoting social inclusion.
Nevertheless, there will be circumstances where being away from work is therapeutic and the most appropriate course of action. Work itself may contribute to poor health for approximately 5-10% of people (Waddell & Burton, 2006). While it is argued that the benefits of work outweigh the risks and harms of long-term unemployment and sickness absence, this nonetheless represents a substantial number of working people and indicates a need for health improvement and health promotion activities in workplace settings. It is clear that work per se is not necessarily what determines health, but the nature and quality of work (See section 10).
Social stratification
Material conditions in particular (which include - but are not solely defined by - income) are key social determinants of health. When examining the relation of income to health, it is not only the income of individuals that has to be taken into account, but also the wealth of the community. If a country is poor, a small increase in per capita income can make a big difference to health. For example, several sub-Saharan African countries have a GDP less than $1000 per capita, and a life expectancy of 45 years or less - mainly due to high levels of child mortality. Poor material conditions (sanitation and malnutrition) being the primary contributor. However, once a country is rich enough to be able to provide the basic material conditions for good health, a larger national income is unlikely to provide better health for the population as a whole. When comparing such countries there is no significant gradient in the relation between income and health. This relationship between income and health as measured by life expectancy is diagrammatically represented in Figure 3 below. Developed societies are represented in historical epochs, but it is possible to think about present day underdeveloped countries as similar in several ways to developed countries at the beginning of the last century, where small increases in income bring about significant life expectancy gains.
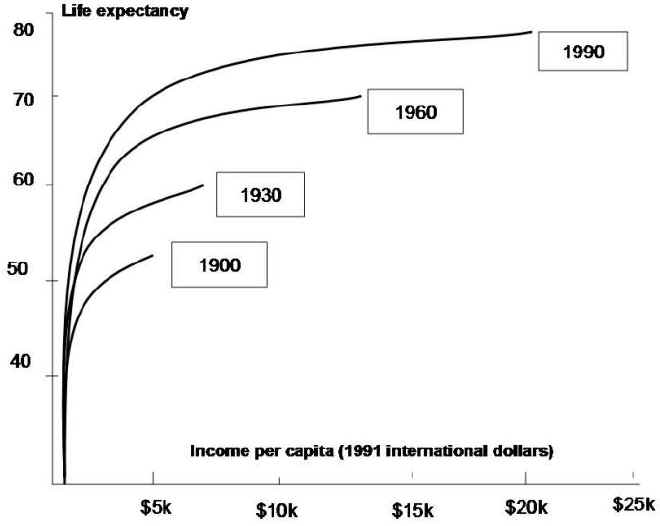
Figure 3: Life expectancy and income per capita for selected (developed) countries & periods (Wilkinson, 1996)
Wilkinson (1996) has argued that a society that tolerates or encourages high income inequality will have poorer health. The existence of wide income gaps between social groups in a developed society has consequences for health, not so much because of material deprivation but because of their psychosocial effects. That is, a society with wide gaps between rich and poor produces low levels of social cohesion. The psycho-social processes associated with this lack of social cohesion ultimately affect the health of all, rich and poor alike. This is because the poor become socially marginalised and are therefore less likely to adhere to the norms of that society, resulting in greater levels of crime and personal violence. These are societies where high proportions of the population are in some way excluded from full social participation, and that do not value all their people equally highly (Marmot:2004). By way of contrast, more egalitarian societies, even with relatively lower per capita incomes, have better health than 'richer' countries. These outcomes are reflected in Figure 4 below. However, it is important to note that Cuba is a clear outlier in terms of GDP and life expectancy, and it is not the case that equal levels of absolute poverty are associated with better health.
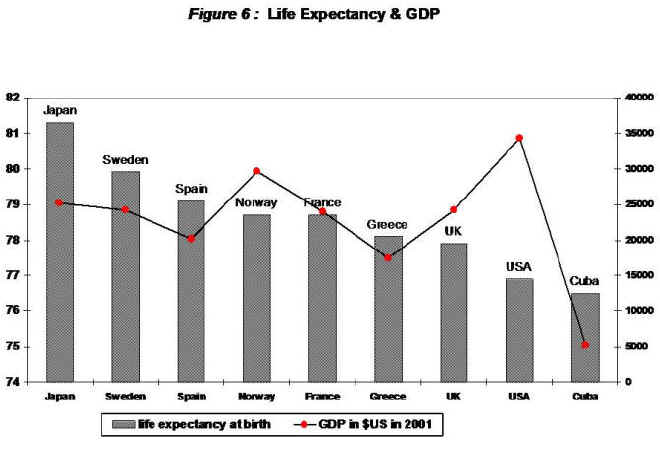
Figure 4: Life expectancy and GDP.
In the relationship between health and income, it is the relative income differences that appear to be more important than absolute living standards in developed societies. Health is therefore related to differences in living standards within these societies, but not to differences between them. In the developed world it is not the richest countries that have the best levels of health, but the most egalitarian ones.
Social Distribution of Disease
Factors that appear to be important explanations for individual health differences, in practice, cannot fully explain the differences in health between social groups within society, or between one society and another. So, for example, it is well-established that a steep gradient in the incidence of coronary heart disease exists between social classes in Britain, and this has been shown to persist after controlling for individual risks of heart disease such as fat consumption and cholesterol levels (Marmot et al., 1991).
In terms of disease patterns, we know that there exists a social distribution of exposure to causative risk factors. Geoffrey Rose (1992) has used this understanding to develop an argument for assessing and tackling these behavioural determinants of the health of individuals at the societal level. He demonstrated that rather than identifying those individuals who are living with a particular disease (with an associated causative health behaviour/risk exposure) as being in a different category than the rest of the ‘normal' population, we should see them as just one end of a population continuum. One of the examples Rose cites to demonstrate this point is high blood pressure. People with hypertension are not a distinct group separate from a normal distribution of blood pressure in society. Rather than having a specific disease/defect not present in the bulk of a population, they actually come within the range of variability described by a bell curve of a normal statistical distribution. After examining the distribution of risk factors for hypertension in a number of different countries at various levels of economic development, Rose concluded that the proportion of people at high risk in any population is simply a function of the average blood pressure, cholesterol levels, etc, in that particular society.
These conclusions concerning the social distribution and determinants of disease cut across the notion of disease as an ‘autonomous individual affliction'. It emphasises that modern diseases and the exposure to the range of causative risk factors are a product of the norms of any particular society.
4. The persistence of Social Inequalities in Health
Policy-makers in pre-war Britain accepted as the norm the existence of large differences in mortality and morbidity levels between the rich and the poor. These differences were seen just as an unfortunate consequence of a market economy. The post-war political enthusiasm for social justice and change that led to the establishment of the British Welfare State, brought about an expectation that social class differences in health would be narrowed following the provision of free comprehensive medical care for the whole population.
Although the general standard of health improved in the post-war years, social class mortality differences failed to narrow. The official view in the mid-1960s was that the cause of these continuing differences in health outcome was behavioural, and that more resources through social policy could not be the solution. But this position ignored research that was available at the time which challenged the notion that the development of welfare state services had succeeded in eliminating disadvantage in access to health and education services, and that low income continued to be a key factor in social disadvantage; the so-called ‘rediscovery of poverty' in Britain.
State health policy from the mid-1970s formally incorporated the strategy of health education, with the aim of convincing the population that it was their own health behaviour, or to use the modern term ‘lifestyle', that required changing. However, this strategy was almost immediately challenged by research being conducted both in the USA and in Britain. The first ‘Whitehall Study' (Marmot et al:1978) found that differences in health behaviours such as smoking, B/P, exercise, and fat intake, were found to account for only a minority of the difference in mortality from CHD between occupational grades. The then Labour government responded by setting up a commission to summarise the evidence for social inequalities in health.
The Black Report (1980) was the first modern official report into health inequity in Britain. It examined the association between social class and health emergent within official statistics, and demonstrated that mortality and morbidity were not randomly distributed throughout the population. The report identified a number of types of possible explanation for this finding:
- Artefact
- Social / natural selection - those with poor health are downwardly mobile.
- Cultural / Behavioural - focus on class differences in health beliefs and behaviour.
- Material circumstances - social differences in income, diet, housing and working environment as key determinants of inequalities in health. This was the explanation accepted by the Black Report (but not by the incoming Conservative government at the time!).
The contemporary picture of health inequalities
Since the publication of the Black Report, there have been a large number of epidemiological studies which have concluded that social class is inextricably linked with social differences in health outcomes. The factors which link social class to health were recognised as reflecting material differences between social groups. These factors include income differences, but are not confined to income. Diet, housing, education, and stressful working conditions, together with what has been termed Social capital (availability of supportive social networks) are all important factors (see Section 11).
The income gap between rich and poor has continued to widen in Britain since the 1980s. Some of the reasons for this trend include a reduction in the real value of state benefits, and a taxation system which favours the well-off (disproportionate number of indirect taxes such as VAT, Fuel etc compared to the more progressive income tax). Britain has some of the lowest wage levels in the E.U, and only relatively recently has the government begun to address the lack of a state childcare system which prevents many women taking-up paid employment.
The evidence for the persistence social class health inequalities in England is cited within the Acheson Report (1998) and more recently the Marmot review (2010).
© I Crinson 2007, Lina Martino 2017
[2] http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/lung-cancer/incidence#heading-Zero
[3]Samaritans: Men and suicide. http://www.samaritans.org/sites/default/files/kcfinder/files/Samaritans_Men_and_Suicide_Report_web.pdf
